In this conversation, “Perimenopause and Mental Health: What to Expect and Solutions for Feeling Better“, Menopause Specialist and Doctor of Nursing Practice, Helen Stearns, DNP, MSCP, joins Reproductive Mental Health Expert, Abigail Burd, LCSW, PMH-C, to break it all down.
Interested in jumping ahead to a specific topic?
Use this list of topics by timestamp to find it, either in the video or in the full transcript below.
0:02 – Introductions and overview of perimenopause, postpartum mental health, and hormones
1:48 – When postpartum mental health overlaps with perimenopause for older mothers
3:40 – Beyond postpartum depression: the role of hormones in perinatal and perimenopausal mental health
4:16 – Who is most at risk for depression, anxiety, and rage during perimenopause
5:11 – ADHD symptoms during perimenopause and their impact on mental health
7:18 – Helen’s personal story: postpartum rage, perimenopause, and mental health as an older mother
9:08 – Perimenopause and rage
10:08 – Strategies and solutions for perimenopausal mental health symptoms
11:47 – What The Menopause Society is and why certification matters
12:39 – Helen’s professional path
15:48 – Hormones aren’t so scary – and could help depression, anxiety and rage in perimenopause
18:42 – Estrogen as a neurotransmitter and its role in mood and anxiety
20:13 – Perimenopause and rage (again)
21:12 – Nervous system reactivity
22:52 – When there is trauma or PTSD plus perimenopause
23:36 – Perimenopause solutions from a Menopause Society Certified Provider
26:51 – Can women in their 30s be in perimenopause?
27:59 – Medical gaslighting in perimenopause
30:13 – Therapy-based solutions for perimenopausal mental health from psychotherapist Abby
31:14 – Avoiding Toxic Positivity
31:38 – Differentiation
34:49 – Somatic approaches for soothing the nervous system and trauma during hormonal shifts
36:30 – HRT = “Husband Replacement Therapy”
36:49 – The Serenity Prayer
37:45 – Signing Off
Full transcript of the video on perimenopause and mental health (with timestamps):
Introductions and overview of perimenopause, postpartum mental health, and hormones
0:02
Abby: All right, welcome. This is Abby from Burd Psychotherapy and I have the pleasure of talking today with a new friend, acquaintance, and colleague named Helen. Helen, could you introduce yourself?
0:13
Helen: Yeah, Abby, thank you for having me here. I’m super excited about talking to you and I just love what we’re about to talk about. So I am a doctor of nursing practice, a nurse practitioner and double board certified in adult geriatric and family care and menopause certified by the menopause society. My jam, my practice, is primarily perimenopausal women, and later than that and earlier than that, with hormone difficulties. I’m so super happy to be here.
0:50
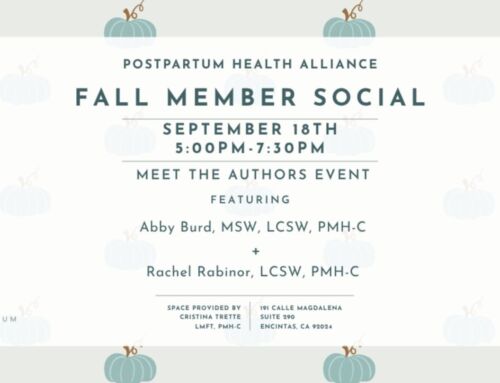
Abby: Awesome. So we recently connected through the San Diego Postpartum Health Alliance. Have you always been interested in perinatal mental health or perinatal health?
1:03
Helen: No, I would say actually that’s not been my focus but it has come into focus both through my own experience of having a child late in life. I had my wonderful daughter at 43 years old and then just connecting with the community and the mental health specialists, the pelvic floor therapists, all who are in this world. I’ve started to really put the pieces together of how our worlds and our patient population, women’s health population interconnects. So that’s become very much in my telescopic view lately.
When postpartum mental health overlaps with perimenopause for older mothers
1:48
Abby&amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;lt;/strong>: When we connected, we started talking about the conversation we wanted to have here today with all of you, which is with more women having children later — something I’ve noticed in my practice and you’ve noticed as well — is that the hormonal changes of postpartum period really just kind of roll into and get confused with the perimenopausal stage. And so it’s like hard to even know the difference. Women are like, “well, I thought I was still having postpartum but I’m now 45 so what does that mean?”</strong>
<strong>2:27</strong>
/>Helen: Yeah, 100% – This is happening to more and more women. In fact, I think this might be now the highest demographic we’ve seen of women having babies now in their 40s or above than we’ve seen at any other time in history. And yeah, it’s very interesting rolling into this perimenopause time. And it’s a very confusing, often very distressing transition as a new mom and then going into perimenopause.
And we can dive into all of these different things, but the mental, emotional health changes that come with hormone fluctuations, the physical changes, it all leads to this huge world of confusion and distress. And that’s kind of why I’ve become very, very passionate about educating women because it’s like you said, “oh, this is just postpartum and while I might have some difficulties, you know, I’ll get through it” and then two years later you’re having the same issues and you’re like, “This isn’t postpartum anymore. What is going on with my body, right?”
Beyond postpartum depression: the role of hormones in perinatal and perimenopausal mental health
3:40
Abby: I think it’s so true. I think when I kind of got into this niche, you know, I was interested in postpartum depression and then I realized it was so much bigger. It was also postpartum anxiety. And then I realized the peripartum stage has so many kinds of hormonal moments that impact our health at so many different stages. For example, I’ve worked with people who were totally fine in the postpartum stage until they stopped breastfeeding and then that weaning created this hormonal shift that made them depressed and suicidal.
Who is most at risk for depression, anxiety, and rage during perimenopause
4:16
Abby: Dr. Leslie Craig, one of the founders of the Postpartum Health Alliance, taught me that folks that have had some kind of postpartum mood or anxiety or folks that are more sensitive to the mood and anxiety impacts of hormonal shifts premenstrual — premenstrual dysphoric disorder, or a premenstrual exasperation, such as somebody who already has a little bit of underlying depression and it gets worse in that premenstrual week. So for any person who’s a little bit more sensitive to those hormones, that perimenopausal stage is really likely to be destabilizing.
4:58
Helen: Yeah, I like that word, destabilizing. And also, I mean, it’s kind of, it sounds dramatic, but it can almost be catastrophic for these women because what’s worked for them before doesn’t work anymore.
ADHD symptoms during perimenopause and their impact on mental health
5:11
Helen: I actually just took a really cool webinar on ADHD and perimenopause. And it was just one more of those mental and emotional conditions that we women are actually very good at compensating, right? We’re very good multitaskers. We hold jobs and families together and ourselves. And it’s one of those things that perimenopause doesn’t cause ADHD. And again, perimenopause doesn’t cause this or this, but it kind of unmasks some of these instabilities.
I think that’s a great word. And medications that used to work don’t work anymore or rhythms and even birth control that you absolutely felt great on, you no longer can even tolerate it. You go crazy on it. I’m really glad we’re talking about this. I’d love to share what I went through.
And then I’d love to dive into some of like the physiology of what’s happening in the peripartum time with hormones and then what’s happening in perimenopause and why there’s actually so many similarities.
6:32
Abby: I’d love for you to tell us your personal story. But before we do that, you said something so apt that the strategies we’ve discovered as adults that work for us just are no longer fitting. And I think we’ll definitely have to make sure to circle back and say what are the new strategies? What’s going to work? Yeah.&amp;amp;lt;/p&amp;amp;gt;&amp;lt;/p&gt;</p>
&amp;lt;p>&amp;
<p>lt;strong&amp;gt;6:57&amp;amp;lt;br /&gt;<strong&amp;amp;gt</p></p></p>
<p><p>;Helen</strong&gt;: Yeah. I love
that. And I would</p>
like to learn from you too a
s a mental health counselor because this can have really huge consequences in how you feel about yours
elf. You know, we internalize a lot of this. We
feel guilty for the reactions that we’re having when a lot of it’s just physiological that’s happening
.</p></p>
<h3&
<p>gt;Helen’s personal story: postpartum rage, perimenopause, and mental health as an older mot
her</h3&gt;
&lt;
strong>
7:18<br />&lt;strong&amp;gt;Helen: My story, just in brief, is that I got pregnant at 42 intentionally and didn’t realize h
ow lucky I was to just have no problems with fertility at that point. I had my baby at 43 and she is the great joy of my life but it definitely took a toll on my mental health, my body. I gained a lot of weight that I could not budge. I was very stressed. I went back to work maybe two months after she was born.</p>
I really d</p>
on’t even think I realized how bad it was until I sort of had this come to Jesus conversation with my husband where he’s just like, “I don’t even wa
nt to come home these days. like you’re just complaining all the time. You’re so negative and you’re just like being negative all the time with me and criticizing me.” And I’m like, “Oh my god.” Like I was like panicking. I thought he was going to leave me.
And I was scrambling for help. And I went to my therapist. I got a psychiatrist. And here I’m a nurse practitioner. I wasn’t embedded in this perimenopausal world at the time, but I really had to get some help for myself. I was desperate.
I was like, “What’s wrong with me?” It’s really hard for women out there and I felt guilty and I was tired and putting a lot of guilt and shame on myself.
A lot of women come to me with these stories.
Perimenopause and rage
<strong>9:08</strong><br />He</strong>len</strong>: I want to talk to you, Abby, about perimenopausal rage — I’ve heard it described as “rage flashes” much like hot flashes where it’s completely unrelated to the level that you should have — terrible anxiety and depression and then you combine it with the classic insomnia that can be a huge component of perimenopause on top of your baby waking you up. Then that’s another thing. Two years later, your baby’s sleeping through the night, but you can’t anymore. You’re like, “the pieces aren’t fitting together right, something’s happening that’s not just postpartum.” It’s very profound with hormonal shifts that are happening.</p></p>
&amp;lt;p>9:50</</strong>strong><br
<p>/><strong&gt;Abby: Wow, Helen, that’s so much. Thank you for sha</h3>
ring that with us. That seems like it was a really challen
ging time. And I’m also hearing you talk about it past tense. And so that gives me hope that you’re no longer at such an intense place.
Strategies and solutions for perimenopausal mental health symptoms
10:08
Helen: Oh, I’m so much better, so much more stable. I got the help I needed. I was able to level out some of my hormones, counseling and I found a women’s health psychiatrist to also help me. I had the resources and really worked on stress management. I learned just small things. I want to encourage our listeners, you can make a big difference.
I’m sure you teach this all the time, but I learned to close my computer during my lunch break. I was a super stressed, busy nurse practitioner and I had so much charting to do and you know the patient loads never ending. I learned to just close my computer, eat my lunch and go outside and take a walk around the block. Little interventions like that made such a big difference. Making sure I was moving my body and hydrating and eating well. Little things like that really helped. Having the resources really helped.
11:21
Abby: That’s so funny that you say that because one of my goals for myself last year was to go outside and walk during the middle of the day. Just the dramatic difference that made in helping my mood throughout the day versus the days where it’s like, “oh, I haven’t been outside all day.”
11:34
Helen: Yeah, I love it. Right. It did. It really did make a big difference for me getting some sunshine. Sometimes I turn my little meditation app on or I would just listen to some music. It was very helpful.
What The Menopause Society is and why certification matters
11:47
Abby: Thank you for sharing with us your story personally. And so, I want to ask a little bit about your story professionally. So, in addition to your DNP as a nurse practitioner, you have MSCP after your name. Could you tell us a little bit about what that means?
12:08
Helen: Yeah. So that’s a certification by the Menopause Society of the United States. So there’s also an international menopause society. And it’s not exactly a board certification as in it’s not a covered entity that does the board certifications, but you do have to pass a certifying exam. I took that last year, but I started my NP career in 2020 at a sexual medicine clinic.
Helen’s professional path
12:39
I’d love to share this story because I think it’s just actually a story of hope for people. I don’t want to sound cliche, but things really do work out. It changed the whole trajectory of my life. I couldn’t find a job at all because I graduated with my doctorate during COVID and everything had been shut down, right?</p>
There were hiring freezes, the clinics were all closed down. They were doing telemedicine and I was getting super anxious and almost panicky and months were going by and I found the sexual medicine opening on some random job website. I have no idea to this day what it was. And I applied. They hired me right away. And it really ended up changing the whole course of my life.</p>
I started seeing women and men with hormonal and sexual medicine concerns, and many young menopausal women. It was profound and fascinating and none of which we had learned</p>
in school. Not a word of this. I don’t even think I had known what a pelvic floor therapist was.</p>
<p>There is just a whole world of women’s health that’s not taught.
It was so fa
<p>scinating to me. I ended up leaving the sexual medicine clinic after about a year when things started opening up because I was really anxious about not losing my primary care skills, which was super important to me to make sure I was really using what I had gone to school for. And I still kept trying to incorporate practices that I had learned. It never left me from the sexual medicine clinic.
<p><p>I was treating women’s urinary issues and sexual pain and doing what I could, getting some push back from assisted living facilities, and a lot of my clients were already very old, 80s, 90s, hundreds and I established wonderful relationships with them but there just started to be this passion in me to treat women in midlife and I saw a whole generation or two of women who through no fault of their own missed out on midlife care because of things like the WHI and hormone fear and we have now learned so much and I was like I have to treat women in midlife. I really want to.
I want to protect your bones and your heart and keep you from getting urosepsis. I had so much passion and as soon as I stepped out and decided I was going to do this I had so much joy. I didn’t think I could do it. I had never wanted to be a business owner, never wanted to own my own practice. Just all these self-limiting beliefs. Things have just opened up and made way and I’m I’m so happy every day I just feel like I’m doing what I love now. So that’s kind of my backstory.
Hormones aren’t so scary – and could help depression, anxiety and rage in perimenopause
15:48
Abby: We were just thinking about how the messages that our mom’s generation got about how estrogen was so scary, so harmful, you had to avoid it. And now everything I’ve learned just has made me very much see that it could be preventative for long-term health. Not only for helping right now with symptoms.
When I look at the research of how many women in their 40s are given an anti-depressant or are treated for depression or anxiety when really the first line should be hormone replacement therapy because that could not only help the mood and anxiety disorders but so much else…
16:30
Abby: For me, one of the things that I thought about was preventing osteoporosis, which I’m at risk for based on my mom’s history, based on my build. And so, just knowing, it’s just kind of like taking your vitamins, taking your calcium, all the things.
16:48
Abby: All right, welcome back. We’re talking with Helen about how hormones can really be first-line ways of treating depression and anxiety in women in the perimenopause stage.
16:58
Helen: Yeah, absolutely. I love that you’re bringing this up because this is something that is so underutilized and this is where a lot of women in the 40-year-old age range are getting gaslit and dismissed by their providers. They are. I’m not bashing anti-depressants or anti-anxiety medications at all. They have their place and they’re very appropriate.
But the data actually shows that hormone therapy during this perimenopausal time can actually be more effective, like you were saying, than anti-depressants. Anti-depressants and anti-anxiety meds shouldn’t necessarily be the first thing that are offered to women when they come for help for hot flashes, sleep and anxiety. One of the first questions we should be asking is maybe they are perimenopausal.
This is one thing that I am absolutely so passionate about and I see this all the time is the mental health issues and my perimenopausal moms that come to me, they’re so distressed by the rage, by the irritability. “I’m having to apologize to my kids all the time. I was never an angry person. I was never anxious, now I’m having panic attacks in the grocery store… where is this coming from?” Right?
And what I like to really leave my events and my consultations with is a message of hope. Like this is not your fault. This is not essentially you, right?
Estrogen as a neurotransmitter and its role in mood and anxiety
18:42
Helen: What this is, Abby, is these are massive hormone fluctuations that are influencing your dopamine, serotonin, and GABA receptors in your brain. And estrogen’s part of its job is actually a neurotransmitter. We have so many estrogen and testosterone receptors in our brain.
Progesterone itself is a huge mood stabilizer that directly influences the GABA receptor which stabilizes our mood and dopamine is our pleasure and our happy receptors.
And so when our bodies are going through these massive up and down with no rhyme or reason, just utter chaos, can you imagine what’s happening in our brains?
And it’s very similar to the postpartum time. This is why it can be somewhat indistinguishable and very confusing. You go from levels of thousands on your estrogen when you’re pregnant to bottoming out.
You have almost no estrogen in your body during lactation in the immediate postpartum time. This is why you can have that hair loss, right? Hair hates hormone changes.
19:50
Helen: That’s why we monitor so closely for postpartum anxiety and depression because of these massive hormone shifts. So again, this is not your fault. This is nothing you are doing. This is real chemical imbalances and fluctuations.
Perimenopause and rage (again)
20:13
Abby: Before we get to the solutions, and we are going to get to the solutions, let’s just talk a little bit about rage, either postpartum rage, or in the perimenopause and menopause stage, because I think that’s where we start to feel like, am I going crazy? Is there something wrong with me? Taking it on personally when we see this disconnect between the activating event and our reaction, right?
And so that’s what feels kind of out of control or I’m not myself. “I’m judging myself. I’m being mean to the people I love most. My children.” That can be so very upsetting.
<p><p><strong>20:52&amp;lt;/strong><br /><strong&gt;Helen: I’m laughing a little bit inside because while it’s not a laughing matter, it’s kind of funny listening to some of the memes or people talking online because it’s like your husband’s breathing too loud or chewing too loud and this is literally what triggers the rage, right?</p>
Nervous system reactivity</h3></h3>
<strong>21:12<b
r /><strong>Abby</strong>: Or sometimes it’s not that, b</h3>
ut sensory sensitivity. Just like ADHD getting activated in the postpartum stage or in menopause, it’s because our sensitivity to sounds and to touch can change.
<p><p>It’s a nervous system reaction. It’s similar to a post-traumatic stress reaction where our nervous system is getting so activated. It’s like the fight or flight response. And so no wonder you feel like fighting! Some people are googling, “Is wanting to murder my husband a sign of perimenopause?” Like yes. Yes it is.
22:03
Helen: No, that’s really interesting, Abby, that you would liken that to post-traumatic stress because that is what it feels like. And I remember like there were times when you know as a mom you’re just touched out like you love your kid more than life itself, but you’re like please like stop touching me. and for me even I get very auditorially over stimulated if someone just talks and talks and talks and talks at me like I want to go out of my mind.
Abby: Or if a show is playing in the background and people are talking .
Helen: It’s very interesting, right, we become very sensitive to stimuli.
When there is trauma or PTSD plus perimenopause
22:52
Abby: And at the same time, I do see a lot of folks who have birth trauma or they’ve gone through infertility or had a very sick infant or had previous trauma or more. And so sometimes there are layers of post-traumatic stress on top of this stage. Yeah.
23:17
Abby: You know, to jump into solutions. There’s a lot we can do to regulate the nervous system and to really develop better control over our reactions.
Does it make sense to kind of hear from your perspective and your discipline what you do and I can talk about ways that I help people?
Perimenopause solutions from a Menopause Society Certified Provider
23:36
Helen: I would love this because I know you and I, Abby, both want this to be a message of hope and practical takeaways. Just knowing you’re not going crazy and that there are things that we can do to stabilize those hormones.
Hormone Therapy in Perimenopause
From a strictly medical standpoint, we can definitely work on stabilizing hormones. But I also like to say along with that is I can throw all the hormones in the world at you, but if we’re not regulating certain physical aspects of your life, they’re not going to be as effective.
Sleep in (peri)menopause
Sometimes it’s a chicken and egg situation as well. “Well, you’re telling me to fix my sleep, but I can’t sleep.” And I’m like, “Oh, okay.” Because this is a hormonal issue. So, sometimes a little bit of hormones can go a long way to fixing the stress levels and the sleep issues.
Treating perimenopause symptoms in lactating new moms
Yet every woman and every situation is very individualized. So, there’s no blanket, oh, this is what’s going to fix you, right? because I don’t want to give you estrogen if you’re lactating. I don’t want to shut down your lactation, right? But there are things that we can do and there are stabilizing things and we would definitely work on sleep and maybe you would benefit from a little bit of progesterone for a mood stabilizer or maybe this is the time where you would benefit from an anti-anxiety medication.
Time for yourself
Also, like you and I were talking about before, is carving that time out for yourself and really that can be very challenging for new moms is really making that a priority and how practically you’re going to do that. I think that’s where people like you come in, Abby, working with the family dynamics and the lifestyle.
“But yeah, hormone therapy”
25:40
Helen: If you’re not immediately in this postpartum time, there’s a lot that we can do to help stabilize these hormones and these moods and the fatigue. And if you’re not lactating, we can work on giving you some estrogen.
Cycling hormone therapy in perimenopause
25:57
And sometimes women only need it cyclically, right? Maybe you’re very young in perimenopause and you might do really well during the luteal phase, which is the week or two leading up to your period when many women start to experience heightened anxiety, increased symptoms like ADHD or increased depression and fatigue.
Vaginal symptoms
26:20
Helen: Something we can always treat though is any kind of sexual pain, vaginal, or vulvar dryness. That is something I would want to know about if I were seeing you and doing an intake with you because that can also cause its own distress physically, emotionally, relationally. Pelvic floor therapy or a localized cream that’s not going to be systemically absorbed can help.
So I hope that helps a little bit. Quite a lot of tools.
Can women in their 30s be in perimenopause?
26:51
Abby: You know, you mentioned about being young in the menopausal stage, but also could we just talk about age range? Because actually, although, we talk classically about women in their 40s, I think that the age range for perimenopausal symptoms can actually be much bigger.
From your standpoint, what do you see in terms of age?
27:16
Helen: Yeah, it’s very normal to see women 35 and above. So late 30s and above. So you are really not in any abnormal class if you start to see perimenopausal symptoms in your 30s. Many women are shocked by this and I’m so glad you brought it up.
I just met with a pelvic floor therapist who had her kids at 36 and 39 and she started noticing symptoms, had no idea what was going on, and basically had to research herself.
Medical gaslighting in perimenopause
27:59
Helen: But I’m so glad you brought that up because that alone can be very reassuring for women. Knowledge is power. Like tuning into your body and realizing, “oh, maybe this is what’s happening.”
28:06
Abby: “Something’s different for me.” I just hear so many cases of what we now call medical gaslighting. Maybe you’re younger. So a woman in her 30s, mid to late 30s is having a provider tell her like, “Oh, no, you’re too young. It can’t be it can’t be perimenopause.” I think so much of it is “trust your gut”. Like trust you. You are the expert on your life.
28:29
Helen: Yes. Trust your intuition. And I also have some information on helping women advocate for themselves with their doctor. We should, you know, we I can send you the links or helpful information. But also another thing I really like to tell my women that I think could be valuable is don’t let your provider also dismiss you by saying your labs are fine.
Many providers just don’t know what else to do besides check labs. And so they see these quote normal hormones. Well, maybe they’re normal on Tuesday morning, but by Thursday night you’re completely bottomed out and different. We do not treat perimenopause based on labs. It’s not helpful. And this is where a lot of women are getting dismissed over and over and over again.
29:20
Abby: Or going somewhere charging an arm and a leg for labs that might not even tell them anything.
Helen: Yes. On the flip side, yes. Do not spend hundreds of dollars on labs that are not validated.
Abby: You diagnose on symptoms, right? You go by how someone is feeling.
Helen: Yes. Yes. This is not to say, carte blanche, labs can’t be helpful in certain situations. Absolutely they are. And I draw my own whole panel. But I don’t even require that before I see you. If I were to see you as a patient, I would go off symptoms, right? I already know what’s happening if you’re telling me you’re having night sweats and hot flashes or you can’t sleep or you’re having new or increased anxiety, I already know. I don’t need labs to tell me.
Do I want to see your thyroid? Yes, I’d like to see different things, but I’m going to treat your symptoms. That’s super crucial for people to understand.
Therapy-based solutions for perimenopausal mental health from psychotherapist Abby
30:13
Abby: Now, if you’d like to kind of hear from my perspective a little bit. My practice, especially in recent years, has focused so much on the nervous system and a somatic focus, looking at the whole body. I love being aware of your whole body and noticing how you’re feeling in the moment and where you’re feeling things.
When I’m working with someone who’s feeling like their reactions are too big, it could be from post-traumatic stress, it could be from hormonal fluctuations, it could be from life stressors, it could be from a lot of reasons.
Avoiding Toxic Positivity
31:14
Abby: Yet if I have someone who’s wanting to work on themself, the first thing I’m going to do is not discount the fact that they’re feeling stressed from the world we’re living in, right? So, I don’t want to be coming from a place of toxic positivity. Because things in life are truly hard. Things in our country are truly hard. Things in their family may be truly hard.
It’s really important that we’re doing both, and… We’re validating what’s real and we’re looking at what we can do to make things better.
Helen: Yep. I love that.
Differentiation
31:38
Abby: So part of it is differentiating, right? Like so a trauma response is okay. So imagine you had a baby in the NICU and there was an alarm bell that would go off because your baby stopped breathing. Then when you go home and your baby is breathing fine, but you hear alarm bells, your nervous system is going to react as though your baby could die. And that’s a very human biological response to our nervous system overgeneralizing.
32:09
Abby: And so our work in therapy is to really tap into your inner wisdom to differentiate, you know, is this specifically a scary time or is this specifically a time to self soothe?
Imagine your house is on fire. Should you sit down and meditate and take deep breaths?
No, you should get up and run away and be in action. So that stress response is giving you those stress hormones to get up and run. Which you do.
There’s a time for action, a time for change, a time to protest, and a time to accept and self soothe.
32:47
Helen: I love that. Yep. Our bodies are very intelligent, you know. We need stress responses to survive. Yeah.
Abby: Right. And there’s times when you hear, historically, this is not just recent. This is like ancient history where women in this life stage are maybe leaving an abusive relationship. It’s that, you know, “I no longer care. I no longer care about society or fitting in a box.” And I think it’s also pretty important to embrace the freedom and the power that comes with this life shift.
33:29
Helen: Yes. I love that so much. I definitely try to give that message as well. Like this is a time of new power, new vitality really. Many women become actually very creative during this time. They come into their own, like you were saying. We don’t care as much about what people think. We realize the life that we want and it’s the time for you to start to embrace that. I love it. People do say the 50s are the golden years and I’m really starting to see why. I’m not quite 50 yet, but I’m looking forward to it.
34:18
Abby: Yeah. Right. If I were working with someone who’s in this life stage, it’s also a time to look at your goals and your values and being intentional in your life that you are living consistent with your values, but also not being so intentional and such an adult that you’re losing your ability to play and to connect with your sense of wonder and, as you said, creativity.
Somatic approaches for soothing the nervous system and trauma during hormonal shifts
34:49
Abby: One of my favorite tools for helping to regulate the nervous system from a polyvagal perspective are Brainspotting, which is a somatic therapy that uses looking in particular directions to tap into places in our brain and to process even without words.
This could be helpful for even preverbal trauma (before we have words) to really be a place of connecting to that healing in the body and that inner wisdom in the body. That’s been a pretty powerful tool that I’ve seen help a lot of people and it’s amazing for rage and hormonal rage of any kind.
35:32
Helen: Beautiful. Beautiful. That’s going to be very helpful. Right. And I love what you said too about like differentiating between whether you do need to leave a situation that’s no longer serving you. And I think that this is so important to talk about because a lot of divorces do happen during this time.
But being able to sort it out with someone like you. Whether this is just hormones with someone like me and you want to divorce your husband because your hormones are going crazy or is it because really this relationship is not healthy and you don’t want to make a decision without that empowerment behind it, right?
I think this is where you and I both come in. Where both sides of our women’s health practice can be so beneficial.
HRT = “Husband Replacement Therapy”
36:30
Helen: Just on a side note, I did hear a podcast that talked about HRT standing for “husband replacement therapy.” Sometimes that’s what it can mean, right? But a lot of times it’s chemical fluctuations.
The Serenity Prayer
36:49
Abby: Well, would it be all right if I leave us with the Serenity Prayer? Have you heard of the Serenity Prayer? I think the Serenity Prayer encapsulates differentiation. I often think that it’s “both, and…” We want to change and challenge injustice, and we want to take care of ourselves.
The Serenity Prayer goes:
Grant me the serenity to accept the things I cannot change, the courage to change what I can, and the wisdom to know the difference.
Helen: So beautiful.
Abby: You have that wisdom. It is inside of you. Trust it.
Helen: Yep, you do.
Signing Off
37:45
Abby: Well, it’s been a pleasure chatting with you, Helen. I’ll be adding all your links and places for people to find you and anything else you’d want to share.
Helen: Yeah, absolutely. Happy to meet with any of you if you have questions for me or just concerns or want to talk about your symptoms. Yeah, I absolutely do free calls. Happy to talk you through some of this stuff.
Abby: All right, take care.





What are your thoughts?